Pancreatitis is inflammation of the pancreas. The pancreas is a long, flat gland that sits tucked behind the stomach in the upper abdomen. The pancreas produces enzymes that help digestion and hormones that help regulate the way your body processes sugar (glucose).
Pancreatitis can occur as acute pancreatitis — meaning it appears suddenly and lasts for days. Some people develop chronic pancreatitis, which is pancreatitis that occurs over many years.
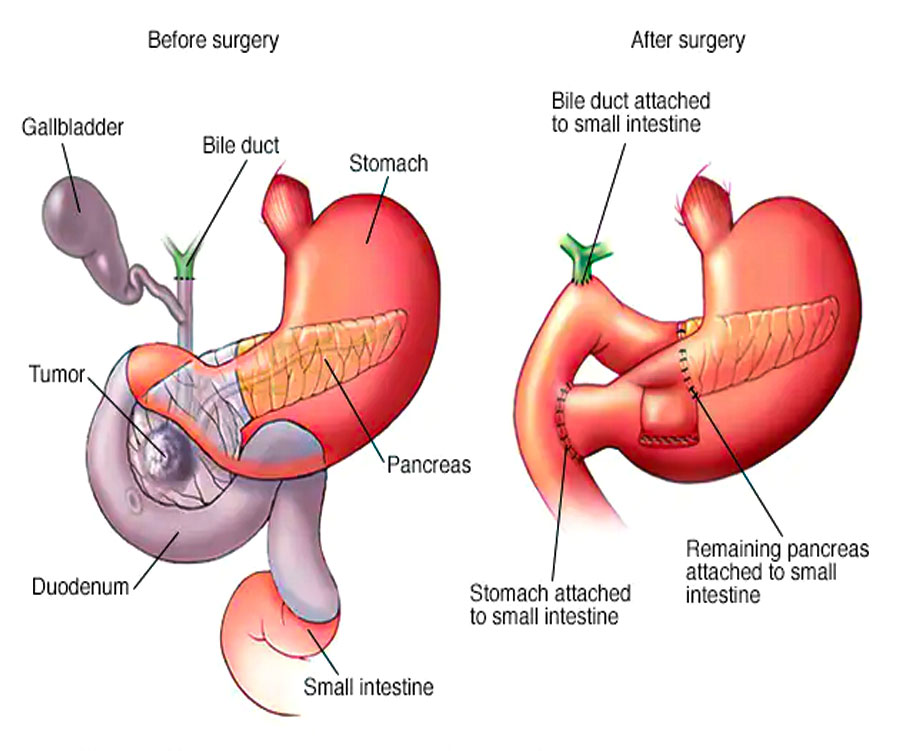
The pancreas surgery is used to treat tumors and other disorders of the pancreas, intestine and bile duct. It is the most often used surgery to treat pancreatic cancer that's confined to the head of the pancreas. After performing the pancreas surgery, your surgeon reconnects the remaining organs to allow you to digest food normally after surgery.
The pancreas surgery is a difficult and demanding operation and can have serious risks. However, this surgery is often lifesaving, particularly for people with cancer.
Once diagnosed, most of the patients requires hospitalization for the management. Mild pancreatitis usually resolves with supportive care, which includes analgesics and intravenous fluids. Moderately severe and severe acute pancreatitis can be potentially life-threatening and requires more extensive monitoring and supportive care. A tube through the nose is often placed for the feeding purpose. Infected fluid collecting around the pancreas, sometimes known as pseudocyst, can be drained endoscopically or by placing a percutaneous drain tube.
ith the proper treatment and in expert hands, most of the patients with acute pancreatitis recover well. Treatment of underlying cause is essential to prevent the recurrence, alcohol should be stopped and gall bladder surgery is performed in patients with stone disease. Raised lipid or calcium levels are controlled by the medications.
MRCP, and Endoscopic Ultrasound (EUS) are the special test to study the pancreas and its duct. EUS provides the excellent information about the pancreas gland and the duct.
Endoscopic Retrograde Cholangio Pancreatography (ERCP) is a special endoscopic technique to treat narrowing in pancreatic duct known as stricture and limited number of small stones. For the large stones in pancreatic duct, a small scope known as pancreatoscope is introduced in the pancreatic duct and ElectroHydraulic Lithotripsy (EHL) energy is used to break the stones.
Extracorporeal Shock Wave Lithotripsy (ESWL) is a technique, where ultrasound and X-ray are used to focus on the stone, which is broken by the use of shock waves. Few patients with chronic pancreatitis may form a fluid collection around the pancreas known as pseudocyst, which may lead to fever, pain abdomen, jaundice and vomiting. EUS guided cystogastrostomy is a safe technique, during which pseudocysts are drained inside the stomach obviating the need of surgery.
In few patients with chronic pancreatitis, a mass may form in pancreas, which may be due to inflammation or tumor formation. Such lesions require extensive evaluation with CT, PET scan and endoscopic procedures. Sometimes sample is obtained through endoscopic ultrasound. Many of these lesions may regress after stopping alcohol and smoking, few of such lesions may require surgery.
Pancreatic Tumor – Smoking, diabetes mellitus, chronic pancreatitis and obesity are the common underlying risk factors of pancreatic cancer. Most common symptoms of pancreatic cancer are upper abdomen pain, jaundice, loss of appetite and weight loss. In patients with high suspicion, CT scan is obtained first, and in case of equivocal results, EUS and tissue sampling may be performed. Around 20% of the cancer are localized and can undergo surgery, rest of the patients are managed by chemotherapy. After chemotherapy, few lesions may regress and become resectable and can undergo surgery. Prior to chemotherapy, ERCP and stenting is often performed to treat the jaundice. During ERCP, stent is placed in the bile duct, to remove the blockade caused by the tumor. Few patients with pancreatic cancer have severe pain, EUS guided CPN (Celiac Plexus Neurolysis) is performed in these patients for the pain relief. Few selected unresectable/ surgically unfit pancreatic tumors can be ablated by a special minimally invasive EUS guided Radio Frequency Ablation (RFA) technique.
Emergence of specialized pancreatic care teams equipped with better understanding of the disease & experience in performing complex endoscopic pancreatic procedures is likely to change the outcome of pancreatic diseases in favourable direction.
Modern pancreatic treatment is based on principle of utilising minimally invasive techniques and can aptly be described as being safe acceptable for the patients.
For most patients, full recovery after pancreas surgery takes about 1 – 3 months. During this time, patients will need to attend all of their follow-up appointments and take care to adjust their eating habits and other routines to allow their healing digestive tract time to acclimate
The primary goal of treatment is to achieve long-term pain relief, maintain nutrition, to slow down the further progression of the disease, control of the complications associated with the disease, and to restore the quality of life. Triggers like alcohol, smoking, and certain drugs should be avoided to prevent further damage to the pancreas.
Good pain management is a very important part of treatment. This includes oral painkillers like NSAIDs, narcotic medications, injectable medications and interventional procedures like celiac nerve blocks. Pancreatic enzyme supplement and avoidance of high fat food are also measures to control pain. These measures are also important from the nutritional point of view.