THINKING CLEARLY
If general anesthesia is given or if you are taking narcotic pain medication,
it may cause you to feel different for 2 or 3 days, have difficulty with
memory, or feel more fatigued. You should not drive, drink alcohol, or make
any big decisions for at least 2 days
NUTRITION
When you wake up, you will be able to drink small amounts of liquid. If you
do not feel sick, you can begin eating regular foods.
Continue to drink lots of fluids, usually about 8 to 10 glasses per day.
Eat a high-fi ber diet so you don’t strain during bowel movements
ACTIVITY
Slowly increase your activity. Be sure to get up and walk every hour or so to
prevent blood clots.
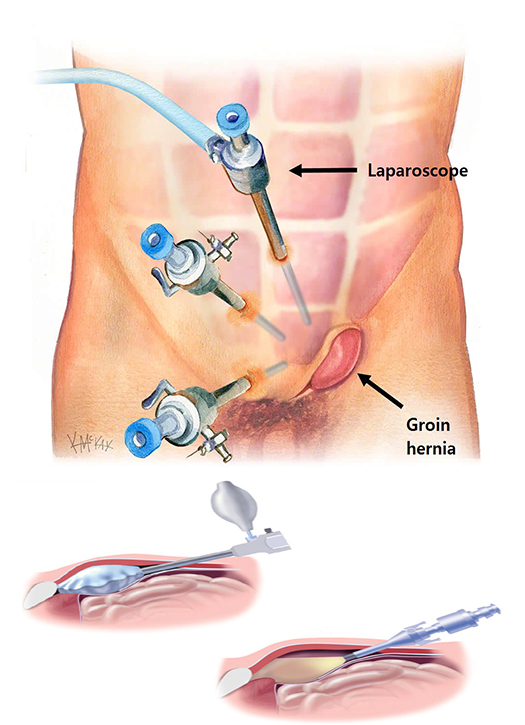
You may go home in 1 to 2 days for a laparoscopic repair. If your appendix
ruptured or you have other health issues or complications, you may stay
longer.
WORK AND RETURN TO SCHOOL
You may return to work after 1 to 2 weeks after laparoscopic or open repair,
as long as you don’t do any heavy lifting.Discuss the timing with your
surgeon.
Do not lift items heavier than 10 pounds or participate in strenuous activity
for at least 4 to 6 weeks.
Lifting limitation may last for 6 months after complex or recurrent hernia
repairs.
WOUND CARE
- Always wash your
hands before and after touching near your incision site.
- Do not soak in a
bathtub until your stitches or Steri-Strips are removed. You may take a
shower after the second postoperative day unless you are told not to.
- Follow your
surgeon’s instructions on when to change your bandages.
- A small amount of
drainage from the incision is normal. If the drainage is thick and
yellow or the site is red, you may have an infection, so call your
surgeon.
- If you have a
drain in one of your incisions, it will be taken out when the drainage
stops.
- If you have a
glue-like covering over the incision, allow the glue to fl ake off on
its own.
- Avoid wearing
tight or rough clothing. It may rub your incisions and make it harder
for them to heal.
- Protect the new
skin, especially from the sun. The sun can burn and cause darker
scarring.
- Your scar will
heal in about 4 to 6 weeks and will become softer and continue to fade
over the next year.
BOWEL MOVEMENTS
Avoid straining with bowel movements by increasing the fiber in your diet
with high- fiber foods or over-the-counter medicines (like Metamucil® and
FiberCon®). Be sure you are drinking 8 to 10 glasses of water each day.
PAIN
The amount of pain is different for each person. Some people need only 1 to 3
doses of pain control medication, while others need more. The new medicine
you will need after your operation is for pain control, and your doctor will
advise how much you should take. You can use throat lozenges if you have
sore throat pain from the tube placed in your throat during your anesthesia.